One of the most annoying side effects that patients suffer after certain prostate cancer treatments is incontinence. This past spring, our very own Dr. Natalya Lopushnyan presented at the 19th Annual Massachusetts Prostate Cancer Symposium where she talked at length about incontinence after prostate cancer treatments.
Below is a condensed version, which includes a discussion around why incontinence happens and what men can do to treat it. As with all content on Greater Boston Urology's blog, the following information is educational in nature, not medical advice. Always talk to your physician about your specific health care questions and conditions.
[Editor's note: This article was reviewed and updated on 5/18/21 with additional links.]
Why does incontinence after prostate cancer sometimes happen?
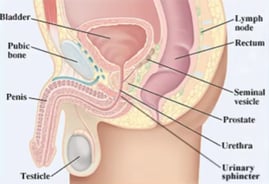
For the prostate, it's all about location. The prostate gland, which looks like a walnut, sits beneath the bladder and envelops the urethra right under the bladder.
Another important structure is a muscle that's called the sphincter; it's right under the prostate. Think of the sphincter muscle like a faucet. When it works well, you don't leak urine because it's closed. You can open and close it whenever you want. But when the sphincter muscle is injured, you will have problems with urination or with leakage. This is why it's all about location. It's not about the prostate gland per se, but where it's located—and what's located near it.
Understanding how the bladder works.
 Remember, the bladder has two functions. The main function of the bladder is to store urine. When you're storing urine, your bladder is relaxed so it can fill up with urine. The little sphincter muscle is closed so you don't leak.
Remember, the bladder has two functions. The main function of the bladder is to store urine. When you're storing urine, your bladder is relaxed so it can fill up with urine. The little sphincter muscle is closed so you don't leak.
When your bladder is full, you go to the bathroom. Your bladder squeezes (it's very important for the bladder to squeeze for you to urinate) and the sphincter muscle relaxes. The "faucet" is open and you can eliminate your urine.
Why does a prostatectomy often result in incontinence?
Prostatectomy is the physical removal of the prostate with surgery. The prostate is removed and because the sphincter muscle is in such close proximity to the prostate, the sphincter muscle might be injured in the process.
Post prostatectomy, the patient has a catheter for 7-10 days. After the urologist removes the catheter, almost all patients leak urine because the sphincter muscle "forgets" how to function for a little while and/or it is injured during surgery.
Again, leakage happens pretty much in everyone right after prostate surgery, but it continues to improve and it may continue to improve for up to a year. The good news: after a year, about 90% of men are dry. This means about 10% still leak and have to either seek other treatments or wear pads.
Note: Medication doesn't help incontinence issues after a prostatectomy. Why? The meds are typically directed at the overactive bladder, meaning the bladder that squeezes too much. That's generally not the problem in men, and that's why they don't work. It's not a bladder issue; it's a sphincter issue.
Why does radiation sometimes result in incontinence?
During radiation, the effects and urinary issues are different. We're not removing the prostate, but we're killing the cells in the prostate with radiation. So the area near the prostate, including the P tube, urethra, and even parts of the bladder, might become irritated from the radiation. This can lead to irritating voiding symptoms: increased frequency, urgency, even blood in the urine. But these symptoms improve once radiation is complete.
Radiation oncologists have gotten so good at their craft that now very little radiation gets on to the bladder or the bowel and these irritating voiding symptoms are much better now than what they were 20, 15, even 10 years ago.
[Editor's note: SpaceOAR Hydrogel can also be an option during radiation treatment.]
What can patients do about incontinence that persists?
Pads. Most patients need to wear pads for a few months after a prostatectomy. But continuing with pads for the long-term is another option.
Kegel exercises and pelvic floor physical therapy. Pelvic floor physical therapy involves strengthening the entire area and addresses much more than simply incontinence (think fecal incontinence, constipation, etc.). Kegel exercises strengthen and train the sphincter muscle to keep you dry. Here's a great how-to from the Mayo Clinic regarding Kegel exercises for men. After a prostatectomy, we will advise patients to do Kegel exercises every single day.
Catheters. In terms of catheters, you could opt for an outside catheter that's worn like a condom and attached to a bag or an internal catheter. An internal catheter is placed into your urethra and all the way up to your bladder. It's held in place by a little balloon inside and it connects to a bag as well. This isn't an ideal solution for most men, since catheters are a device that you have to wear and they may lead to more infections.
Penile clamps. Another device the patient would wear, the clamp provides enough pressure to the urethra to keep it closed.
Surgical options. Surgical options might be appropriate for men who are 6, 12, or 18 months post-treatment, most often prostatectomy, and who still leak a lot of urine (and they've tried Kegel exercises and other pelvic floor physical therapy).
- Bulking agents: Essentially, some form of collagen or similar material is injected inside the urethra to make it more closed. Picture a pipe. If it's open, the liquid will just flow through it, but if we make it narrower, less liquid will leak out. The pros: the procedure doesn't take long to perform, and while it is a surgical procedure, some urologists perform it in their office. The downside is that it doesn't usually give patients 100% satisfaction because most times, it doesn't last that long. Men would have to come back and get it redone.
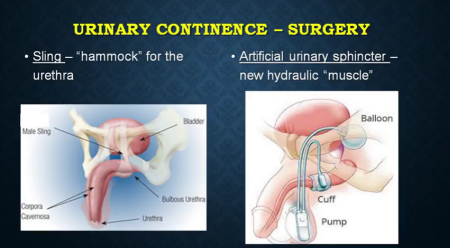
- Sling surgery. A sling is basically a hammock that is implanted under your urethra and compresses it. It's the same idea as above: you have an open pipe, we're going to make it close, and the pipe is going to leak less. It is a good surgical option, and it's a good option for many men, but if the patient leaks excessively, meaning the patient loses every single drop that's in his bladder, this will probably not make the patient completely dry.
- Artificial urinary sphincter. It's a hydraulic device and it requires a surgical procedure to be placed inside your body. It consists of a cuff that goes around the urethra and a little pump that's in the scrotum, not in the testicle. Once it's implanted, in the active form, the cuff is inflated so the urethra doesn't leak. Then when the patient is ready to pee, he goes to the bathroom, pushes a little button, and the cuff opens up and he urinates. After he's done, the cuff closes again about a minute later.
An important final point: not all leakage is the same. Two men who undergo the same prostate cancer treatment and who now deal with leakage might require completely different treatments.
The most important thing patients can do is talk to their urologists about their symptoms. Remember, it may take up to twelve months to fully recover. And the more you leak, the more involved the treatment. But the bottom line: there are options, and your urologist can help you determine the best one for your particular issue.
Are you struggling with side effects from prostate cancer treatment? Let us help.
Make an appointment with one of our world-class urologists to discuss your options.
